Types of Pelvic Inflammatory Disease: Causes and Stages Explained
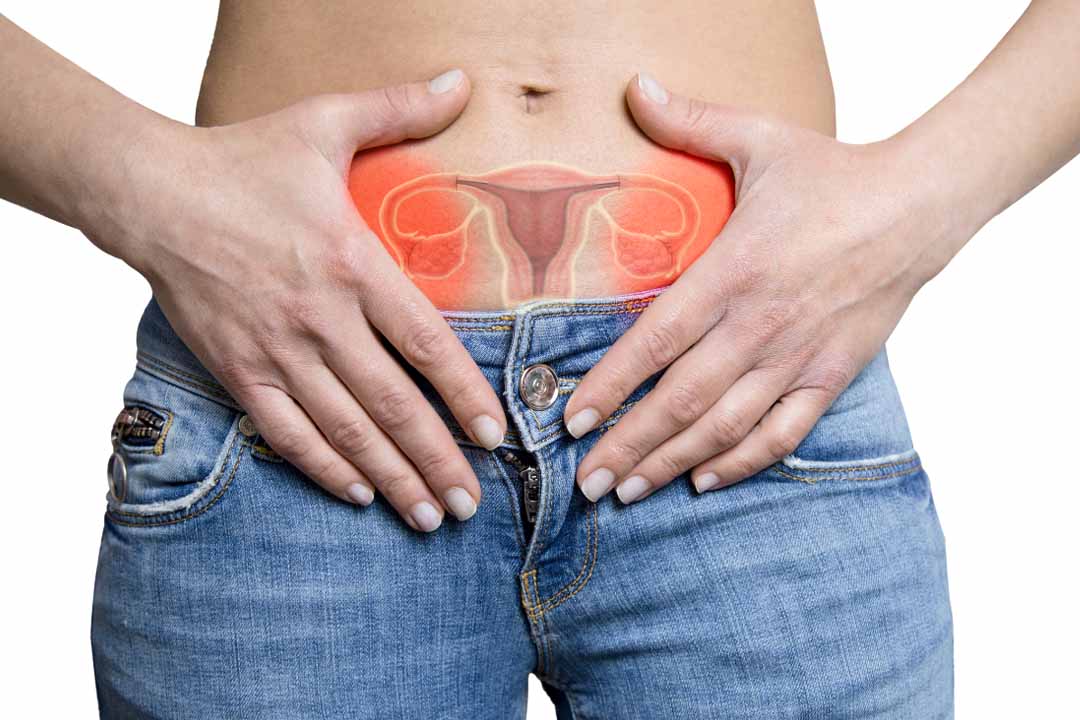
Pelvic inflammatory disease, often called PID, is an infection that affects a woman’s reproductive organs. It usually begins when bacteria travel upward from the vagina into the uterus, fallopian tubes or ovaries. Many women do not notice symptoms in the early stage, which is why the condition sometimes remains undiagnosed for a long time. When left untreated, PID can lead to long term problems such as difficulty getting pregnant or ongoing pelvic pain.
Most issues can be avoided with early care and suitable treatment. Patients can identify symptoms earlier and seek medical attention at the right time if they are aware of the many forms of pelvic inflammatory disease. In addition to discussing recovery, treatment choices and frequently asked questions, this article provides a detailed explanation of the main types of PID.
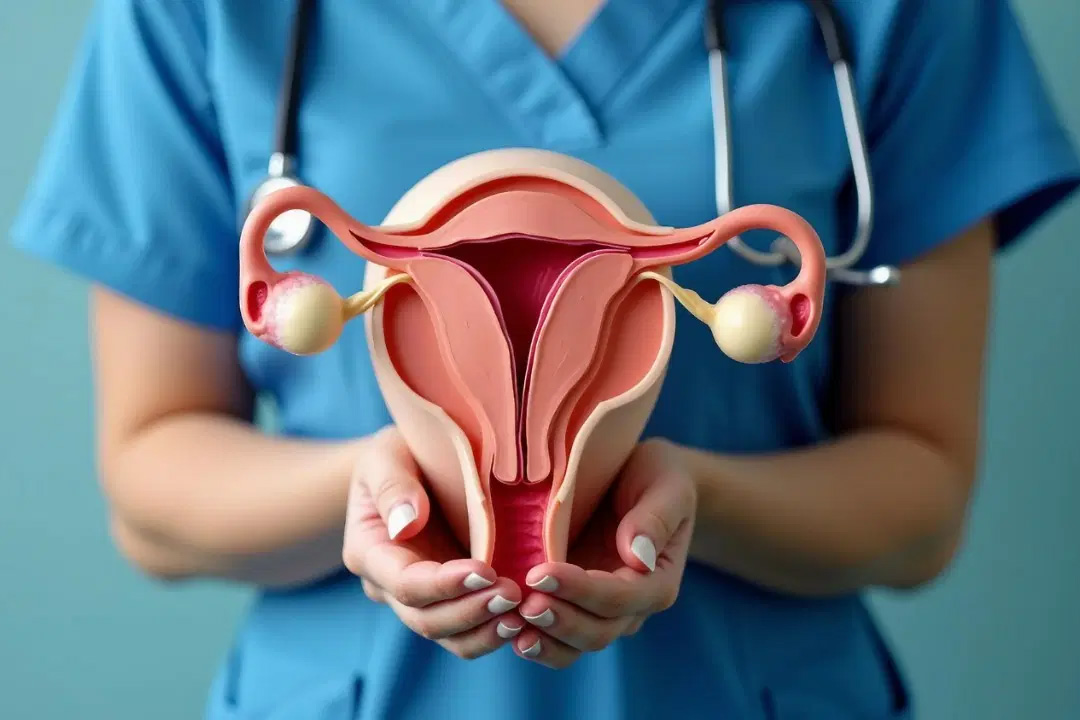
What is Pelvic Inflammatory Disease?
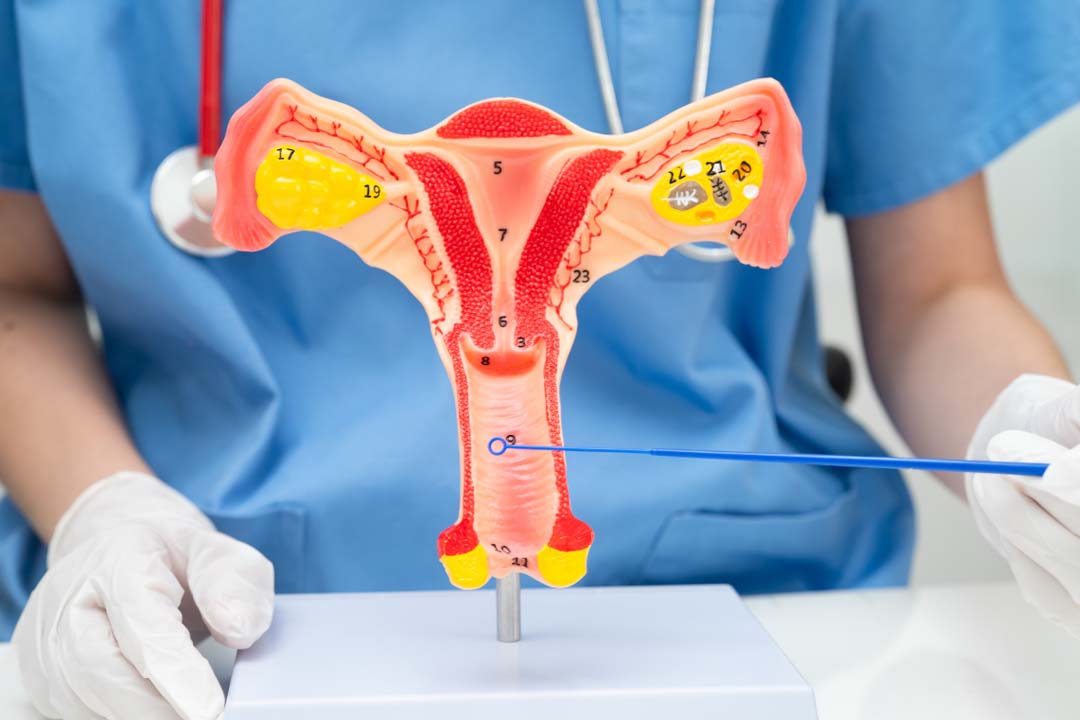
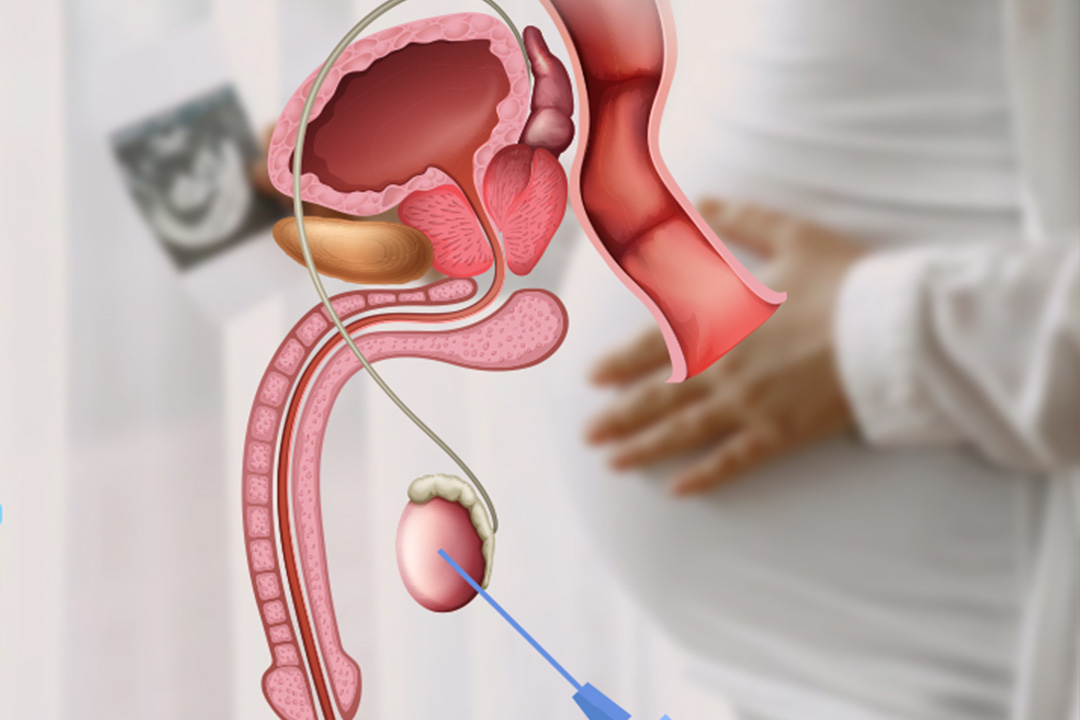
Pelvic inflammatory disease is an infection of the upper female reproductive organs. It can involve the uterus, fallopian tubes, and ovaries. In most cases, bacteria linked with sexually transmitted infections move from the vagina into deeper reproductive organs.
Common symptoms may include lower abdominal pain, unusual discharge, fever, pain during sex, or irregular bleeding. However, some women do not notice any symptoms at all. Because signs can be mild or hidden, many people only discover PID later when they experience fertility problems or chronic pelvic pain.
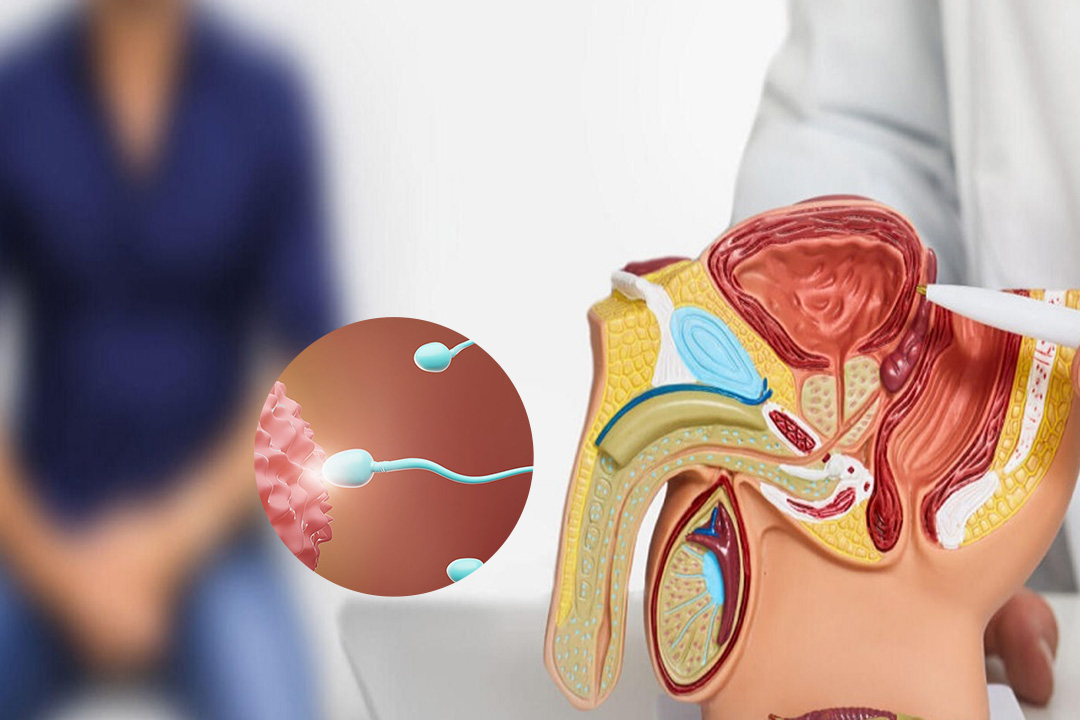
Why does PID develop?
Pelvic Inflammatory Disease (PID) develops when bacteria, primarily from sexually transmitted infections (STIs) like chlamydia and gonorrhea, travel upward from the vagina or cervix into the uterus, fallopian tubes and ovaries. This infection causes inflammation, which can lead to severe damage, scarring, and long-term complications.
Primary Causes and Factors for Development
- Sexually Transmitted Infections (STIs): The leading cause (up to 90% of cases) is untreated bacterial STIs, specifically Chlamydia trachomatis and Neisseria gonorrhoeae.
- Normal Vaginal Bacteria: Sometimes, bacteria naturally present in the vagina can spread upward, particularly if the natural balance is disturbed.
- Unprotected Sex and Multiple Partners: Increased risk of exposure to infections.
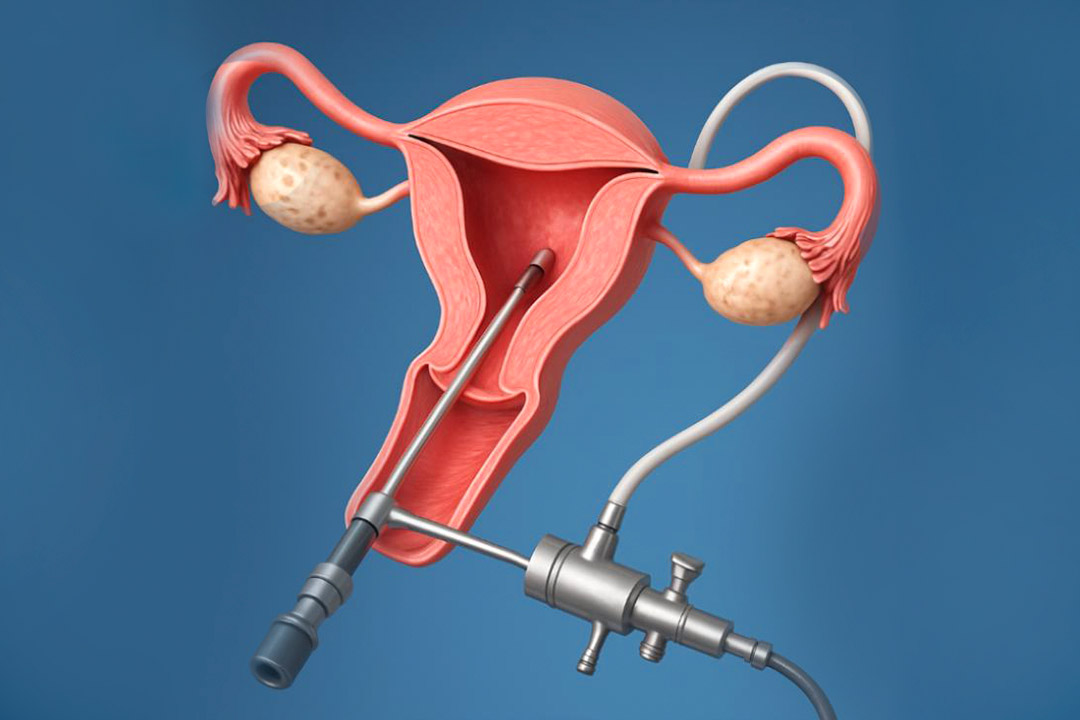
- Medical Procedures: Procedures that pass through the cervix, such as insertion of an Intrauterine Device (IUD) (highest risk in the first few weeks), or following childbirth, miscarriage, or abortion.
- Douching: Douching is the practice of washing or cleaning out the inside of the vagina with water or cleansing mixtures, a practice health experts strongly advise against. Regular douching can force bacteria into the upper genital tract and disrupt natural vaginal flora, raising the risk of infection.
- History of PID: A previous episode of PID makes a woman more susceptible to future infections.
Types of Pelvic Inflammatory Disease
Doctors often classify PID based on how the infection behaves, how severe it is and how long it has been present.
Acute Pelvic Inflammatory Disease
Acute PID means the infection develops suddenly and causes noticeable symptoms. Women with acute PID often experience pelvic pain, fever, discharge, or pain during intercourse. Symptoms can range from mild discomfort to severe pain.
This stage usually occurs when bacteria rapidly spread from the lower genital tract to the uterus or fallopian tubes. If treated early, most patients recover without long term damage.
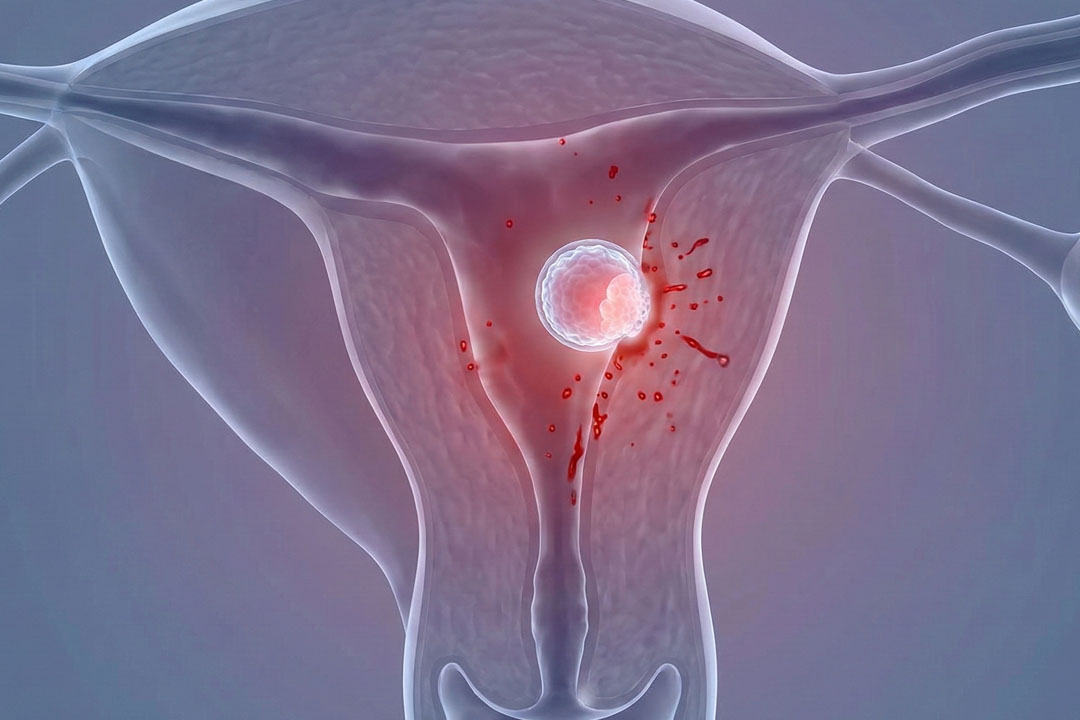
However, ignoring symptoms can increase the risk of infertility or ectopic pregnancy because inflammation may harm the fallopian tubes.
Chronic Pelvic Inflammatory Disease
Chronic PID refers to long standing inflammation that develops over time. It often occurs when an earlier infection was mild, untreated, or not fully cleared. Women may not have strong symptoms but can experience persistent pelvic pain or discomfort.
Scar tissue formation is common in chronic cases. This scarring can lead to ongoing pain during ovulation or intercourse and may affect fertility.
Because symptoms are subtle, many women seek medical care only after facing repeated pain or difficulty conceiving.
Subclinical Pelvic Inflammatory Disease
Subclinical PID means the infection is present without obvious symptoms. Some women do not notice any pain or discharge, yet inflammation still damages reproductive organs.
Doctors often detect this type during fertility evaluations or routine screening. Even without clear symptoms, untreated infection can still lead to tubal damage or infertility.
This form highlights why regular screening for sexually transmitted infections is important for sexually active individuals.
Mild, Moderate and Severe PID
Healthcare providers also classify PID based on severity.
Mild to Moderate PID
Mild to moderate disease usually presents with manageable symptoms such as lower abdominal pain and discharge. These cases often respond well to oral or injectable antibiotics and can be treated without hospital admission.
Severe PID
Severe PID involves intense pain, high fever, vomiting, or signs of abscess formation. Hospital treatment with intravenous antibiotics may be necessary.
Severe infection increases the risk of complications such as tubo ovarian abscess, which is a collection of pus in the reproductive organs.
PID with Tubo Ovarian Abscess
This is a complicated form of pelvic inflammatory disease. An abscess is a pocket of infected fluid that develops in the fallopian tube or ovary. It can cause severe pain and fever and may become life threatening if it bursts.
These cases often require hospital care and stronger antibiotic combinations. Sometimes drainage or surgery becomes necessary.
Treatment Options for Pelvic Inflammatory Disease
Early treatment is the most important step to prevent long term damage. PID is mainly treated with antibiotics.
Doctors usually prescribe a combination of medicines because multiple types of bacteria may be involved. Treatment often begins immediately, even before test results arrive, to prevent complications. Patients should complete the full course even if symptoms improve within a few days.
Typical outpatient treatment for mild to moderate PID may include an injection followed by oral antibiotics for about 14 days. One commonly used approach combines:
- A cephalosporin injection
- Doxycycline tablets
- Metronidazole tablets
This combination helps cover the most common bacteria including chlamydia, gonorrhea, and anaerobic organisms. Doctors may adjust medicines based on test results or patient response.
When is hospital treatment needed?Hospital care may be required if symptoms are severe or complications are suspected. Patients may receive intravenous antibiotics if they:
- Are pregnant
- Have severe infection
- Have an abscess
- Do not improve with oral medicines
Once symptoms improve, treatment often continues with oral medication to complete around two weeks of therapy.
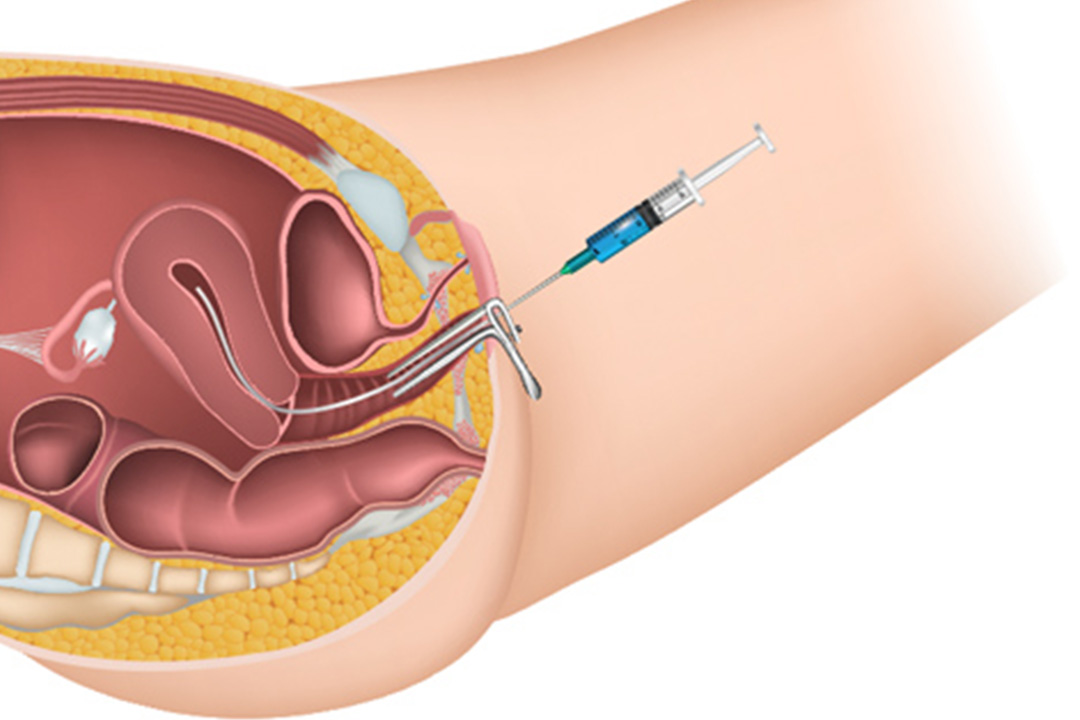
Role of Surgery in PIDSurgery is rarely needed. Doctors may recommend it if an abscess does not respond to antibiotics or if it threatens to rupture.
Procedures may involve draining infected fluid or removing damaged tissue to prevent further spread.
Treating the PartnerPartners should also receive evaluation and treatment. This step helps prevent reinfection because many sexually transmitted infections do not show symptoms.
Doctors usually advise avoiding sexual activity until treatment is complete and symptoms have cleared.
Follow Up and RecoveryFollow up within a few days helps confirm that treatment is working. If symptoms do not improve within 48 to 72 hours, doctors may reassess the diagnosis or change medicines.
Early treatment reduces the risk of complications such as infertility, chronic pelvic pain, or ectopic pregnancy.
Possible Complications if PID is Ignored
Untreated PID can lead to long term reproductive health problems. These may include:
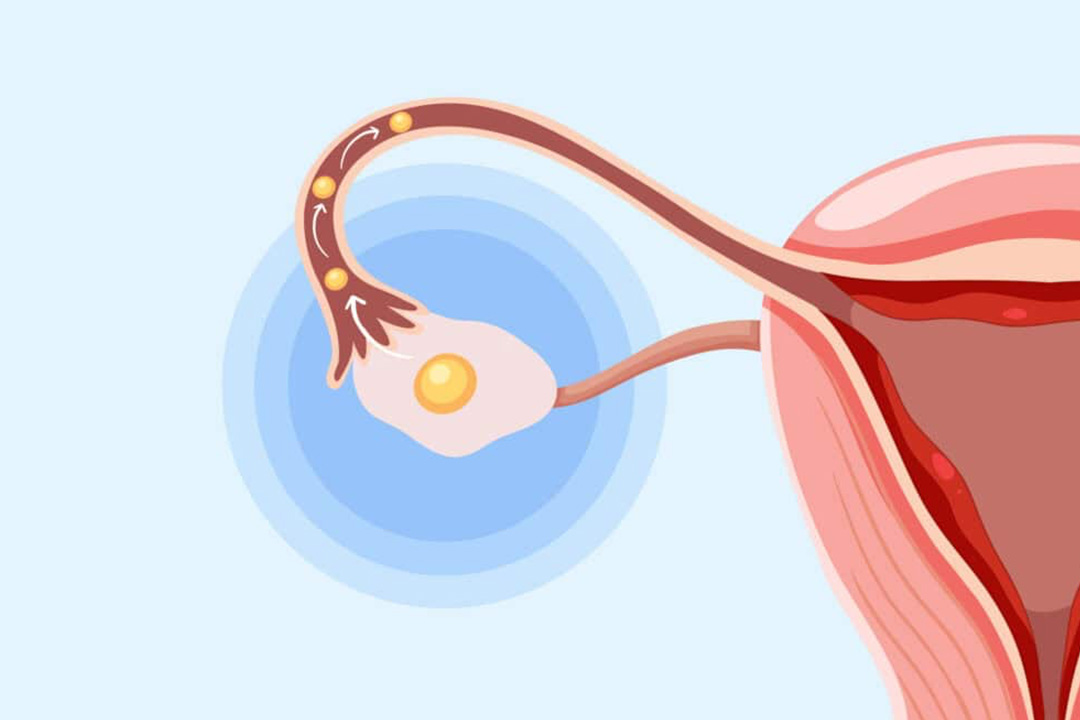
- Infertility due to damage to fallopian tubes
- Chronic pelvic pain
- Ectopic pregnancy
- Abscess formation
The risk increases with repeated infections or delayed care.
Can Pelvic Inflammatory Disease Be Prevented?
Yes, many cases can be prevented with simple steps. Using barrier protection during sex, limiting multiple partners, and getting regular screening for infections can reduce risk.
Early treatment of sexually transmitted infections also helps prevent bacteria from spreading upward into reproductive organs.
Recovery depends on how early treatment begins and how severe the infection is. Most women with mild disease recover completely with antibiotics. Severe or repeated infections may cause long term discomfort or fertility issues.
Following medical advice, completing medicines and attending follow up visits improves outcomes and lowers the chance of recurrence.
Frequently Asked Questions
Can pelvic inflammatory disease go away on its own?
No. PID usually requires antibiotics. Without treatment, infection can damage reproductive organs and lead to infertility or chronic pelvic pain.
How long does PID treatment usually take?
Most antibiotic courses last about 14 days, though symptoms often improve within a few days after starting treatment.
Can I get pregnant after having PID?
Yes, many women conceive after treatment, but repeated or severe infections may affect the fallopian tubes and reduce fertility.
Is hospital admission always required for PID?
No. Mild or moderate cases are often treated at home with medicines. Severe infection, pregnancy, or abscess may require hospital care.
Can PID come back again?
Yes. Reinfection can happen if partners are not treated or if new infections occur. Safe sex and regular screening help reduce risk.
Conclusion
Pelvic inflammatory disease is a common yet often overlooked infection that can affect long term reproductive health. Understanding its types such as acute, chronic, and subclinical forms helps people recognise symptoms early and seek timely care. Most cases respond well to antibiotics when treated promptly. Delayed treatment increases the chance of complications like infertility or chronic pain. Regular screening, safe sexual practices and partner treatment play a key role in prevention.
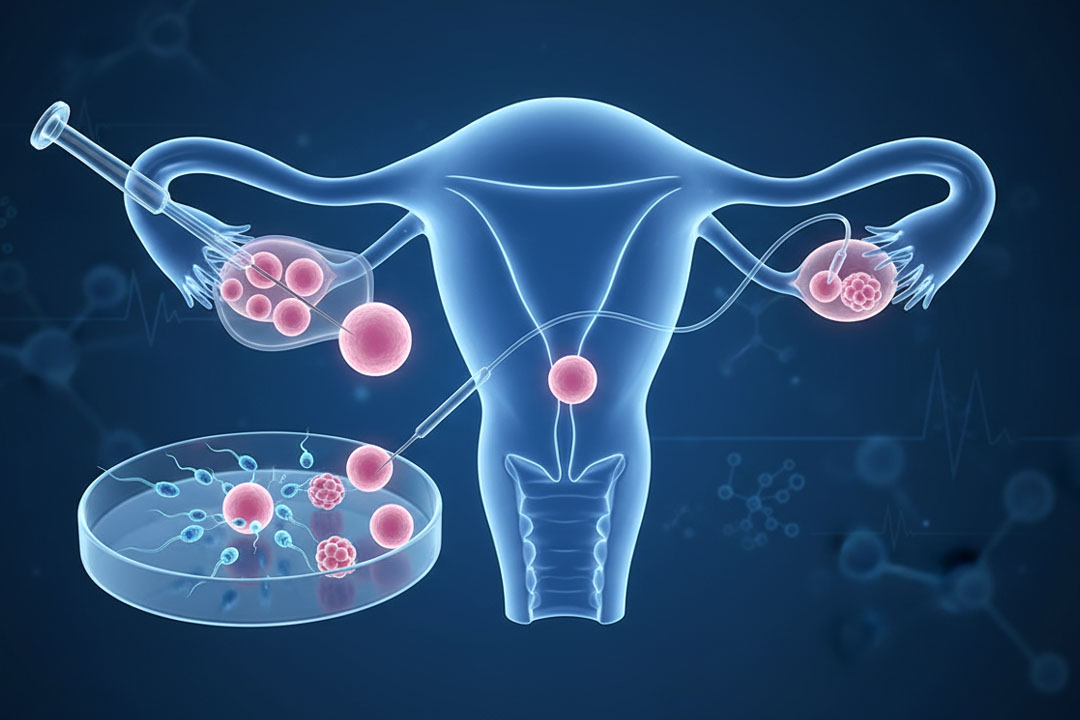
About Us
AKsigen IVF is a premier center for advanced fertility treatments, with renowned fertility experts on our team. Specializing in IVF, ICSI, egg freezing, and other cutting-edge reproductive technologies, AKsigen IVF is committed to helping couples achieve their dream of parenthood. With personalized care and a patient-first approach, AKsigen IVF provides comprehensive fertility solutions under one roof.